151 questions match your search.
An apneic adult is receiving an oxygen flow of 4 L/min through a rigid bronchoscope. After five minutes of apnea, which of the following findings is most likely?
- (A) A decrease in cardiac output
- (B) A decrease in pulmonary vascular resistance
- (C) A decrease in SpO2 from 99% to 89%
- (D) An increase in PaCO2 of 18 mmHg
- (E) Serum bicarbonate concentration of 30 mEq/L
Prior to occlusion of any major pulmonary blood vessels during a thoracotomy, applying positive end-expiratory pressure to ventilation through the dependent lumen of a double-lumen tube and occluding the upper lumen of the tube will
- (A) increase blood flow to the dependent lung
- (B) increase the alveolar-arterial oxygen tension difference
- (C) override hypercarbic pulmonary vasoconstriction
- (D) improve the patient's oxygenation
- (E) increase the right ventricular dP/dt
Initiation of positive pressure mechanical ventilation is LEAST likely to decrease cardiac output in patients with which of the following conditions?
- (A) Abdominal distention with decreased lung volume
- (B) Acute cardiogenic pulmonary edema
- (C) Chronic obstructive pulmonary disease
- (D) Flail chest following an automobile accident
- (E) 20% Right pneumothorax
Which of the following is the most likely cause of a decrease in end-tidal carbon dioxide tension during general anesthesia with a constant minute ventilation?
- (A) Administration of sodium bicarbonate
- (B) Intravenous administration of hypertonic glucose solution
- (C) Decrease in cardiac output
- (D) Decrease in fresh gas flow in a Bain circuit
- (E) Malfunction of the inspiratory valve in a circle system
Syringe A contains 100 ml of normal blood with a PO2 of 2 mmHg, and syringe B contains 100 ml of normal blood with a PO2 of 98 mmHg. The contents of the two syringes are mixed anaerobicaily to equilibrium. The PO2 of the resultant mixture Is
- (A) 27 mmHg
- (B) 50 mmHg
- (C) 63 mmHg
- (D) 96 mmHg
- (E) 100 mmHg
A 70-kg, 22-year-old man who is unconscious after a closed head injury is to undergo emergency splenectomy. He is anesthetized with thiopental, given pancuronium for paralysis, and started on nitrous oxide and oxygen 50% each with controlled ventilation (tidal volume 700 ml, rate 10/min). Pulse is 70 bpm, blood pressure is 160/100 mmHg, PaO2 is 65 mmHg, PaC02 is 45 mmHg, and pH is 7.30. In adjusting the ventilator at this time, which of the following is most appropriate?
- (A) Add 10 cmH2O positive end-expiratory pressure (PEEP), increase respiratory rate to 14/min
- (B) Add sufficient PEEP to increase PaO2 to 80 mmHg
- (C) Add 10 cmH2O PEEP, increase FlO2 to 1.0
- (D) Increase tidal volume to 1000 ml, increase FiO2 to 1.0
- (E) Increase tidal volume to 1200 ml, decrease respiratory rate to 8/min
The acute onset of hypotension without a decrease in mixed venous oxygen saturation is most likely associated with the onset of
- (A) hemorrhage
- (B) myocardial infarction
- (C) pulmonary edema
- (D) pulmonary embolus
- (E) sepsis
Pulsus paradoxus is commonly seen during anesthesia in patients with each of the following conditions EXCEPT
- (A) severe asthma
- (B) right-sided heart failure
- (C) hypovolemia
- (D) atrial septal defect
- (E) obesity
Positive end-expiratory pressure is effective for treatment of hypoxia resulting from each of the following EXCEPT
- (A) cardiogenic pulmonary edema
- (B) intraoperative Trendelenburg position
- (C) lateral position during total hip replacement
- (D) lung contusion
- (E) status asthmaticus
Following a right lower lobectomy, a patient develops a bronchopleural fistula and becomes hypoxic. He is orally intubated and mechanically ventilated with pure oxygen. PaO2 is 65 mmHg, PaCO2 is 70 mmHg, and pH is 7.25. Which of the following will produce the most favorable change in the blood gases?
- (A) Increasing ventilatory frequency
- (B) Increasing suction on the chest tube
- (C) Applying 10 cmH2O positive end-expiratory pressure
- (D) Using a double-lumen tube for differential ventilation
- (E) Starting negative-pressure ventilation
An 8-year-old child with chronic renal failure is scheduled for an operation to create an arteriovenous fistula. Laboratory studies include: Hemoglobin 6.5 g/dl, Blood gases (breathing air) : PaO2 97 mmHg, PaCO2 29 mmHg, pH 7.30 Sodium 129 mEq/L Potassium 5.5 mEq/L Chloride 101 mEq/L Bicarbonate 15 mEq/L. Before inducing general anesthesia, which of the following abnormalities should be corrected?
- (A) Anemia
- (B) Metabolic acidosis
- (C) Potassium concentration
- (D) Anemia, metabolic acidosis, and potassium concentration
- (E) None of the above
Which of the following statements concerning functional residual capacity is true?
- (A) It decreases linearly during a three-hour anesthetic
- (B) It decreases in pregnancy primarily because of a decrease in the expiratory reserve volume
- (C) It increases in patients with a history of heavy smoking
- (D) It increases with pulmonary contusions
- (E) It is smaller (ml/kg) in children than in adults
In a 65-year-old man, which of the following findings on preoperative pulmonary function testing is associated with the highest risk for respiratory insufficiency following pneumonectomy?
- (A) Maximum voluntary ventilation at 65% of predicted
- (B) Mean pulmonary artery pressure of 28 mmHg
- (C) Predicted postoperative forced expiratory volume in one second (FEV1) of 800 ml
- (D) Residual volume to total lung capacity (RV/TLC) ratio of 0.35
- (E) Vital capacity of 3 liters
Which of the following statements regarding carbon monoxide poisoning is true?
- (A) Breathing 100% oxygen at 1 atmosphere reduces the carboxyhemoglobin half-life
- (B) Effective treatment includes administration of methylene blue
- (C) It is commonly associated with respiratory acidosis
- (D) It is incompatible with a normal Sp02 while breathing room air
- (E) The oxyhemoglobin dissociation curve is shifted to the right
After tracheal extubation, a healthy 21-year-old man has a 30-second episode of laryngospasm with marked intercostal and sternal retractions, which are corrected with continuous positive airway pressure administered by mask. He now has dyspnea and tachypnea, and a roentgenogram of the chest shows diffuse bilateral interstitial edema. The most likely cause is increased
- (A) airway reactivity
- (B) intrapleural pressure
- (C) left ventricular afterload
- (D) right ventricular preload
- (E) transpulmonary vascular pressure
A 95-kg, 65-year-old woman receives sevoflurane and pancuronium during a laparoscopic cholecystectomy. Three minutes after administration of neostigmine 5 mg and atropine 1.2 mg, the twitch height returns to normal. Spontaneous tidal volume is 500 ml when the endotracheal tube is removed. In the PACU she reports dyspnea and appears distressed. Which of the following is the most likely cause of the respiratory distress?
- (A) Atelectasis
- (B) Cholinergic crisis
- (C) Pain
- (D) Residual enflurane
- (E) Residual muscle paralysis
A 50-year-old woman develops stridor 10 hours after undergoing thyroidectomy. The most appropriate management is administration of which of the following drugs?
- (A) Albuterol
- (B) Calcium chloride
- (C) Ipratropium bromide
- (D) Racemic epinephrine
- (E) Triiodothyronine
A healthy, spontaneously breathing, supine, anesthetized patient has a PaCO2 to PetCO2 difference of 3 mmHg. Following institution of mechanical ventilation the value increases to 12 mmHg. The most likely cause of this change is
- (A) cephalad displacement of the diaphragm
- (B) decreased production of carbon dioxide
- (C) increased cardiac output
- (D) increased shunting of blood through dependent lung zones
- (E) increased ventilation of nondependent lung zones
Which of the following is the most appropriate initial management of a patient with hypotension secondary to sepsis?
- (A) Calcium chloride
- (B) Corticosteroids
- (C) Crystalloid infusion
- (D) Dopamine
- (E) Fresh frozen plasma
Cessation of smoking on the day prior to an operation is associated with a perioperative
- (A) decrease in carbon monoxide in blood
- (B) improvement in ciliary beating in the airways
- (C) decrease in sputum volume
- (D) decrease in the need for postoperative ventilatory support
- (E) decrease in the risk of deep vein thrombosis
Mismatching of ventilation to perfusion in the lung is greatest in which of the following situations?
- (A) Awake patient, spontaneous ventilation, lateral decubitus position
- (B) Anesthetized patient, controlled ventilation, supine position
- (C) Anesthetized patient, controlled ventilation, lateral decubitus position
- (D) Anesthetized patient, controlled ventilation, sitting position
- (E) Anesthetized patient, spontaneous ventilation, prone position
During a cardiac arrest with effective chest compression and positive-pressure ventilation, 50 mEq of sodium bicarbonate is administered. Which of the following is the most likely result?
- (A) Decreased mixed venous pH
- (B) Decreased SpO2
- (C) Increased PetCO2
- (D) Increased plasma lactate concentration
- (E) Increased serum potassium concentration
You are called to a witnessed cardiac arrest where cardiopulmonary resuscitation is being performed. After successful intubation, arterial blood gas values are PaO2 86 mmHg, PaCO2 63 mmHg, and pH 7.25 at an FiO2 of 1.0. The most appropriate management at this time is to
- (A) repeat arterial blood gas analysis using a new specimen
- (B) administer sodium bicarbonate
- (C) administer fluid challenge with 500 ml of normal saline solution
- (D) hyperventilate the patient
- (E) add positive end-expiratory pressure
Which of the following statements concerning relationships among alveolar pressure, volume, and surface tension is true?
- (A) Surface tension of surfactant decreases as alveolar volume decreases
- (B) Surface tensions of water and of surfactant behave similarly as volume decreases
- (C) Changes in alveolar surface tension with volume are the same during expansion as during contraction
- (D) Pressure in the alveolus is inversely related to surface tension
- (E) Pressure in the alveolus is directly related to alveolar radius
A woman with chronic obstructive pulmonary disease is extubated and minimally responsive after isoflurane anesthesia. She is receiving oxygen 6 L/min through a face mask. Respirations are 10/min, PaO2 is 68 mmHg, PaCO2 is 54 mmHg, and pH is 7.28. The most likely cause of the respiratory acidemia is
- (A) blunted sensitivity to low pH in the medullary respiratory center
- (B) chronic carbon dioxide retention
- (C) decreased lung volume from supine positioning
- (D) depression of carotid body chemoreceptors by halothane
- (E) suppression of hypoxic ventilatory drive by supplemental oxygen
Following pneumonectomy, a paralyzed patient being mechanically ventilated has the following arterial blood gas values: PaO2 71 mmHg, PaCO2 55 mmHg, pH 7.29. SvO2 is 45%. The most likely explanation for this SvO2 is
- (A) decreased red cell mass
- (B) high cardiac output
- (C) hypothermia
- (D) peripheral left-to-right arteriovenous shunt
- (E) ventilation / perfusion mismatch
Each of the following increases arterial to end-tidal carbon dioxide tension difference EXCEPT
- (A) addition of positive-end expiratory pressure
- (B) deliberate hypotension
- (C) endobronchial intubation
- (D) hypovolemia
- (E) pulmonary embolism
An anesthetized, paralyzed patient is placed in the lateral position and mechanically ventilated. End-tidal PCO2 is 34 mmHg and PaCO2 is 43 mmHg. This gradient
- (A) increases during spontaneous breathing
- (B) indicates increased dead space ventilation
- (C) is caused by increased intrapulmonary shunt
- (D) reflects inhibition of hypoxic pulmonary vasoconstriction
- (E) results from increased cardiac output
The carbon dioxide/ventilation response curve
- (A) is primarily a measure of the integrity of the peripheral chemoreceptors
- (B) shows parallel displacement to the left in the presence of opioids
- (C) is linear between a PaCO2 of 20 and 120 mmHg
- (D) shows progressive changes in slope with increased doses of halogenated anesthetics
- (E) is unaffected by a decrease in PaO2 to 60 mmHg
Which of the following statements best describes the decrease in functional residual capacity that accompanies the induction of general anesthesia?
- (A) It does not change compliance
- (B) It is greater with spontaneous ventilation than with controlled ventilation
- (C) It is independent of body position
- (D) It is not corrected by application of positive end-expiratory pressure
- (E) It occurs within the first 10 minutes of anesthesia
Which of the following is the most likely beneficial effect of hyperbaric oxygen therapy in a 24-year-old scuba diver with decompression sickness?
- (A) Decreased production of carbon dioxide
- (B) Decreased size of gas bubbles
- (C) Increased functional residual capacity
- (D) Reversal of membrane pressure effects
- (E) Shift of the oxyhemoglobin dissociation curve to the left
A sensory level of T2 is achieved after administration of spinal anesthesia. Which of the following lung volumes is LEAST likely to be affected?
- (A) Expiratory reserve volume
- (B) Inspiratory reserve volume
- (C) Inspiratory capacity
- (D) Tidal volume
- (E) Vital capacity
For any given FiO2 and PaCO2, the PaO2 is lower in a healthy paralyzed patient anesthetized with isoflurane than in the same patient unanesthetized and breathing spontaneously. The primary cause of this difference is
- (A) controlled ventilation
- (B) increased airway resistance
- (C) inhibition of hypoxic pulmonary vasoconstriction
- (D) intraoperative hypothermia
- (E) preferential ventilation of nondependent lung
A patient is undergoing thoracotomy in the lateral position. Five minutes after initiation of one-lung ventilation using a double-lumen tube and 100% oxygen, SpO2 decreases from 100% to 65%. Which of the following is the most appropriate initial step in management?
- (A) Adding continuous positive airway pressure to the nondependent lung
- (B) Adding positive end-expiratory pressure to the dependent lung
- (C) Increasing the tidal volume to the dependent lung
- (D) Resuming two-lung ventilation
- (E) Verifying the position of the double-lumen tube
Which of the following changes in pulmonary function best explains the more rapid rate of rise of alveolar concentration of volatile anesthetics in pregnant women than in nonpregnant women?
- (A) Decreased functional residual capacity
- (B) Decreased dead space ventilation
- (C) Increased cardiac output
- (D) Increased oxygen consumption
- (E) Increased pulmonary venous admixture
Blind nasotracheal intubation is contraindicated in the presence of
- (A) a basilar skull fracture
- (B) a comminuted mandibular fracture
- (C) an orbital blow-out fracture
- (D) an unstable cervical spine fracture
- (E) a zygomatic arch fracture
If minute ventilation is held constant, which of the following is LEAST likely to alter PaCO2?
- (A) General anesthesia
- (B) Hypothermia
- (C) Increased dead space
- (D) Increased pulmonary shunt
- (E) Induced hypotension
A 60-kg 25-year-old woman is undergoing laparoscopy in the Trendelenburg position during general anesthesia. Five minutes after peritoneal inflation, the peak airway pressure required to deliver a tidal volume of 800 ml increases from 25 cmH2O to 60 cmH2O. SpO2 decreases from 100% to 80% and systolic blood pressure increases from 110 mmHg to 140 mmHg. Which of the following is the most likely cause?
- (A) Acute tension pneumothorax
- (B) Excessively steep Trendelenburg position
- (C) Excessive ventilator tidal volume setting
- (D) Kink in the endotracheal tube
- (E) Massive carbon dioxide embolism
Which of the following findings differentiates the pickwickian syndrome from morbid obesity?
- (A) Carbon dioxide retention
- (B) Upper airway obstruction
- (C) Decreased forced expiratory volume
- (D) Increased shunt fraction
- (E) Increased functional residual capacity
Measurement of which of the following provides the most reliable information about the severity of bronchospasm?
- (A) Diffusing capacity
- (B) Expiratory reserve volume
- (C) Forced expiratory volume in 1 second
- (D) Residual volume
- (E) Total lung capacity
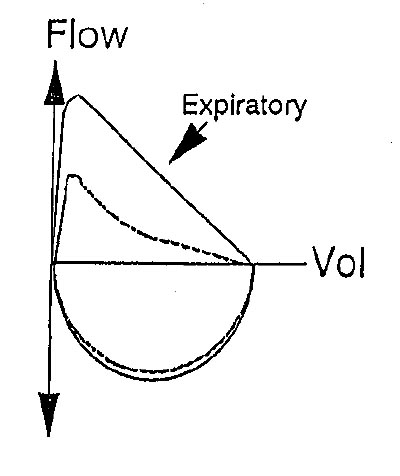
The graphs shown illustrate various respiratory patterns in a patient who is breathing spontaneously with continuous positive airway pressure. Which of the following patterns is associated with the LEAST work of breathing?
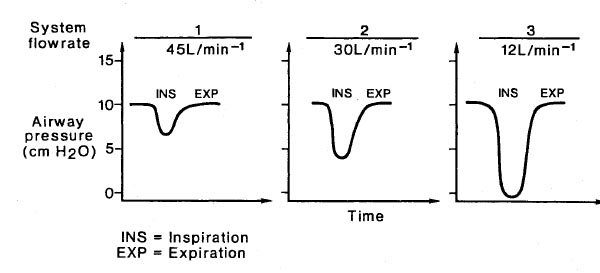
- (A) 1
- (B) 2
- (C) 3
- (D) All patterns are associated with equal work
- (E) There is not enough information to answer the question
Two days after myocardial infarction involving the left anterior descending coronary artery, a patient's blood pressure decreases acutely from 125/80 to 70/40 mmHg, heart rate increases from 75 to 90 bpm, pulmonary artery pressure increases to 50/30 mmHg, and urine output decreases from 60 to 10 ml/hr. Thermodilution cardiac output has increased from 4 to 7 L/min. The most appropriate action is to
- (A) compare mixed venous oxygen saturation in the right atrium and pulmonary artery
- (B) draw blood for culture and start antibiotic therapy
- (C) start dopamine infusion in low dose
- (D) administer a fluid challenge
- (E) monitor peripheral capillary oxygenation by transcutaneous oximetry
A combined epidural and general anesthetic is used for aortofemoral bypass surgery. Just prior to extubation, the patient received morphine 5 mg through the epidural catheter. Eleven hours later, he is unresponsive while breathing 40% oxygen from a face mask. Respiratory rate is 6/min and SpO2 is 92%. Arterial blood gas analysis shows PaO2 80 mmHg, PaCO2 84 mmHg, and pH 7.16. Which of the following statements concerning this patient is true?
- (A) Hypercarbia is contributing to the decreased level of consciousness
- (B) Naloxone is ineffective for reversing the respiratory depression
- (C) The oxygen saturation is higher than expected because of the pH
- (D) The risk for respiratory depression would have been lower with subarachnoid administration of 0.5 mg morphine
- (E) Residual local anesthetic is contributing to the respiratory depression
A 55-year-old man is undergoing craniotomy in the sitting position. Mean arterial pressure is 75 mmHg; arterial blood gas values are PaCO2 41 mmHg and pH 7.37. End-tidal CO2 is 7 mmHg. Which of the following is the most likely cause of the increased PaCO2 to PetCO2 gradient?
- (A) Decreased cardiac output
- (B) Endobronchial intubation
- (C) Hyperinflation of the lungs
- (D) Partial disconnect of the capnograph sample tubing
- (E) Venous air embolism
If a patient with chronic obstructive pulmonary disease is uncooperative during pulmonary function testing, the most accurate assessment of his disease will be derived from the
- (A) forced expiratory volume in 1 second
- (B) forced midexpiratory flow
- (C) forced vital capacity
- (D) maximal voluntary ventilation
- (E) peak flow rate
The trend plot shows end-tidal gases measured during a radical neck dissection. The event occurring at A is most likely
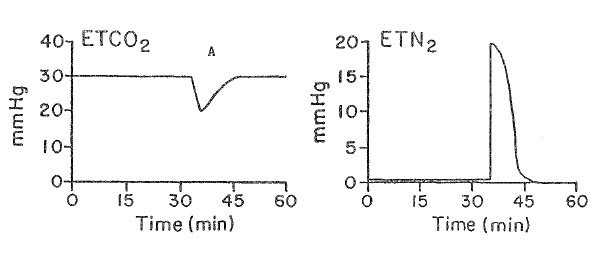
- (A) acute hypotension
- (B) endobronchial intubation
- (C) kinking of the endotracheal tube
- (D) rupture of the endotracheal cuff
- (E) venous air embolism
A computer program for hemodynamic calculations has the following input values: body surface area, arterial blood pressure, heart rate, pulmonary artery occlusion pressure, pulmonary artery pressure, and cardiac output. Each of the following values can be derived with this program EXCEPT
- (A) cardiac index
- (B) stroke volume index
- (C) systemic vascular resistance
- (D) pulmonary vascular resistance
- (E) left ventricular stroke work index
Five minutes after initiating one-lung ventilation using a double-lumen endobronchial tube, a 70-year-old patient has a decrease in Sp02 from 99% to 90%. Tidal volume and respiratory rate are unchanged. Fiberoptic bronchoscopy verifies appropriate positioning of the tube. Which of the following is the most likely cause of the desaturation?
- (A) Blood flow to the nondependent lung
- (B) Failure of hypoxic pulmonary vasoconstriction in the dependent lung
- (C) Inadequate filling of the bronchial cuff
- (D) Inadequate minute ventilation
- (E) Surgical manipulation of the nondependent lung
A 1-month-old infant becomes hypoxemic faster during apnea than an adult. Which of the following is the primary cause of this difference?
- (A) Functional residual capacity in an infant is half that of an adult
- (B) Metabolic rate in an infant is twice that of an adult
- (C) Resting PaO2 in an infant is lower than that in an adult
- (D) The number of alveoli in an infant is 12% the number in an adult
- (E) The hemoglobin dissociation curve in an infant is shifted to the right
The adult oxyhemoglobin dissociation curve will resemble that of the fetus in the presence of
- (A) increased 2,3-diphosphoglycerate concentration
- (B) chronic anemia
- (C) hyperthermia
- (D) metabolic alkalemia
- (E) hyperkalemia
After the bronchial and tracheal cuffs of a right endobronchial tube are inflated, ventilation through the tracheal lumen is not possible. This finding is most consistent with
- (A) cuff occlusion of the right upper lobe bronchus
- (B) intubation of the left bronchus
- (C) left-sided tension pneumothorax
- (D) overinflation of the bronchial cuff
- (E) positioning of both cuffs in the trachea
In a patient with hypovolemic shock, which of the following factors is the best measure of the overall balance between oxygen supply and demand?
- (A) Arterial oxygen content
- (B) PetO2
- (C) Mixed venous oxygen saturation
- (D) PaO2
- (E) Transcutaneous oxygen tension
A 65-kg 70-year-old man in the PACU is breathing spontaneously at 20/min through an endotracheal tube connected to a T-piece with a fresh gas flow of 5 L/min. He has a tidal volume of 350 mL and an FiO2 of 0.5. SpO2 decreases from 98% to 84% over one hour, then improves to 92% with an FiO2 of 1.0. Which of the following is the most likely cause of the hypoxemia?
- (A) Decreased functional residual capacity
- (B) Increased dead space ventilation
- (C) Inhibition of hypoxic pulmonary vasoconstriction
- (D) Room air admixture during inspiration
- (E) Shivering
The flow-volume loop shown is most likely from a patient with which of the following?
- (A) Bilateral vocal cord paralysis
- (B) Chronic bronchitis
- (C) Tracheal stenosis six months after a previous tracheostomy
- (D) Tumor of the lower trachea
- (E) Normal respiratory status
A patient undergoes thoracotomy in the lateral decubitus position. Which of the following maneuvers is most likely to increase PaO2 during one-lung ventilation?
- (A) Applying continuous positive airway pressure to the nondependent lung
- (B) Applying positive end-expiratory pressure to the dependent lung
- (C) Increasing inspiratory flow rate
- (D) Increasing the tidal volume
- (E) Increasing the ventilatory rate
A 30-year-old woman is undergoing laparoscopic tubal ligation. Thirty minutes after induction of general anesthesia, arterial oxygen saturation has decreased to 89%. Arterial blood gases at an FiO2 of 1.0 are PaO2 63 mmHg and PaCO2 40 mmHg; PetCO2 is 32 mmHg. Which of the following is the most likely cause?
- (A) Carbon dioxide embolus
- (B) Endobronchial intubation
- (C) Hypoventilation
- (D) Inadvertent application of high levels of positive end-expiratory pressure
- (E) Leak in the capnography sampling catheter
During rapid-sequence induction prior to an emergency surgical procedure, a 20-year-old patient vomits gastric contents containing particulate matter. An endotracheal tube is easily inserted and ventilation with pure oxygen is initiated. Despite the presence of bilateral breath sounds, SpO2 is 90%. Which of the following is the most appropriate next step?
- (A) Administration of broad-spectrum antibiotics
- (B) Intravenous administration of high-dose methylprednisolone
- (C) Bronchial lavage with normal saline solution
- (D) Bronchoscopy to remove particulate matter
- (E) Cancellation of the surgical procedure
Each of the following findings is characteristic of restrictive lung disease EXCEPT
- (A) decreased elasticity of the lungs
- (B) decreased FEV1/FVC ratio
- (C) decreased inspiratory reserve volume
- (D) increased work of breathing
- (E) normal anatomic dead space
The hemodynamic changes shown would most likely result from infusion of
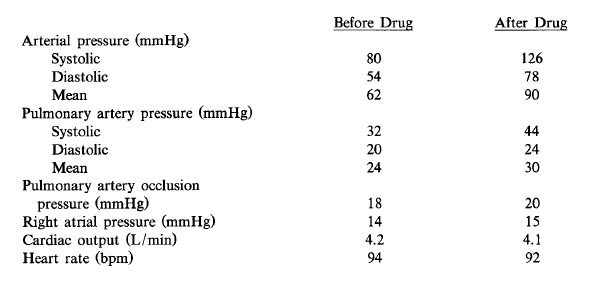
- (A) dopamine
- (B) epinepherine
- (C) dobutamine
- (D) norepinepherine
- (E) isoproterenol
The illustration depicts flow-volume loops for the same person at two different times in his life. Which of the following is indicated by the dotted loop?
- (A) Bronchial tumor
- (B) Chronic asthmatic bronchitis
- (C) Morbid obesity
- (D) Paralysis of a vocal cord
- (E) Subglottic stenosis
During apneic oxygenation (FiO2 1.0) through a rigid bronchoscope
- (A) duration of the procedure is limited by the increase in PaCO2
- (B) functional residual capacity decreases 5%/min
- (C) PaO2 remains unchanged for the first 5 minutes
- (D) PaCO2 increases 2 to 6 mmHg/min for 15 minutes and then reaches a plateau
- (E) PaO2 and PaCO2 equilibrate with mixed venous gases at the same rate
Which of the following results in decreased mixed venous oxygen saturation?
- (A) Cardiogenic shock
- (B) Decreased metabolic rate
- (C) Increased cardiac output
- (D) Left-to-right intracardiac shunt
- (E) Pulmonary vasodilation
A previously healthy 28-year-old man is admitted to the emergency department with a probable opioid overdose. Arterial blood gas values are: PaO2 49 mmHg, PaCO2 76 mmHg, and pH 7.12 while breathing room air. Which of the following statements is true?
- (A) Aspiration of gastric contents must have occurred
- (B) Hypoventilation alone can explain the acidosis and hypoxemia
- (C) The hypoxemia is probably due to noncardiogenic pulmonary edema
- (D) Naloxone should be administered only if the patient is normothermic
- (E) Pure oxygen is contraindicated
Which of the following is the most likely cause of the increased incidence of right ventricular failure in patients with morbid obesity?
- (A) Chronic hypoxia
- (B) Chronic silent pulmonary aspiration
- (C) Chronic silent subendocardial ischemia
- (D) Decreased vital capacity
- (E) Increased pulmonary blood flow
A 30-kg patient with asthma is receiving general anesthesia and being mechanically ventilated with a measured tidal volume of 300 mL. Increasing the fresh gas flow from 3 L/min to 9 L/min without changing the ventilatory rate or I:E ratio will result in
- (A) decreased physiologic dead space
- (B) increased delivered tidal volume
- (C) increased end-expired carbon dioxide
- (D) unchanged delivered minute volume
- (E) unchanged peak inspiratory pressure
A 20-kg, 5-year-old boy under treatment for five days for a cerebral contusion not requiring an operation is still unconscious. After three days of mechanical ventilation, humidified oxygen 40% via T-tube is started. Arterial blood gas analysis shows PaO2 120 mmHg, PaCO2 44 mmHg, pH 7.48, and base excess +6. A nasogastric tube is in place and draining to gravity. Daily fluid therapy has been 5% dextrose in 0.5 normal saline solution 500 ml and 5% dextrose in lactated Ringer's solution 500 ml. Serum electrolyte concentrations are sodium 140, potassium 3.2, and chloride 91 mEq/L. Serum osmolality is 300 mOsm/L. Urine output averages 15 ml/hour. Dexamethasone 8 mg/day has been the only drug therapy. This patient most likely requires
- (A) additional intravenous fluids
- (B) furosemide diuresis
- (C) administration of ammonium chloride
- (D) reinstitution of mechanical ventilation
- (E) administration of potassium chloride
Alveolar dead space is decreased by
- (A) halothane anesthesia
- (B) positive end-expiratory pressure
- (C) deliberate hypotension
- (D) atropine premedication
- (E) decreased tidal volume
At extubation performed one week after nasotracheal intubation, each of the following is likely to occur EXCEPT
- (A) upper airway obstruction
- (B) aspiration after extubation
- (C) ulceration of vocal cords
- (D) tracheal stenosis
- (E) sinusitis
The flow-volume loop indicated by the "X" is characteristic of
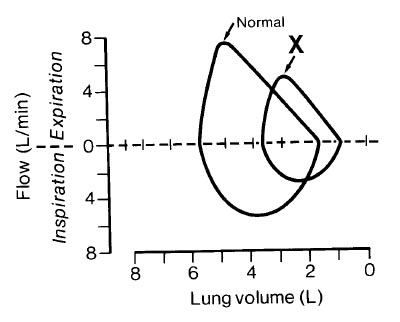
- (A) asthma
- (B) bronchiectasis
- (C) emphysema
- (D) pulmonary fibrosis
- (E) tracheal stenosis
Carbon dioxide retention first occurs when the ratio of forced expiratory volume in 1 second to vital capacity (FEV1/VC) decreases below
- (A) 15%
- (B) 35%
- (C) 50%
- (D) 65%
- (E) 75%
During craniotomy in the sitting position, end-tidal carbon dioxide tension suddenly decreases. Ventilatory excursion of the chest is normal. Further evaluation is most likely to show a decrease in
- (A) alveolar-to-arterial oxygen tension difference
- (B) alveolar-to-arterial carbon dioxide tension difference
- (C) dead space ventilation
- (D) pulmonary artery pressure
- (E) pulmonary artery occlusion pressure
One hour after an open cholecystectomy, a 42-year-old patient is hemodynamically stable and breathing spontaneously (rate 10/min and regular) at an FiO2 of 0.4. Fentanyl, isoflurane, nitrous oxide, and pancuronium were used during the procedure. Analysis of arterial blood gases (pH, pCO2, pO2) is most likely to show:
- (A) 7.18 40 100
- (B) 7.18 60 140
- (C) 7.28 50 85
- (D) 7.40 26 220
- (E) 7.40 40 40
Systemic hypothermia to 30°C is accompanied by
- (A) a shift to the right of the oxyhemoglobin dissociation curve
- (B) a decrease in carbon dioxide dissolved in plasma
- (C) a decrease in the glomerular filtration rate
- (D) an increase in MAC of volatile inhalation agents
- (E) low-voltage, high-frequency EEG pattern
Postoperatively, a patient is being mechanically ventilated by a constant-flow, pressure-cycled ventilator with the following initial settings: inspiratory/expiratory (I/E) ratio of 1:2, peak inspiratory pressure (PIP) of 25 cmH2O, and rate of 10/min. One hour later, the I/E ratio is 1:4. Which of the following would ensure that the minute ventilation is the same as that initially set?
- (A) Inflate the endotracheal tube cuff to prevent leakage
- (B) Double the respiratory rate
- (C) Decrease the expiratory pause until the I/E ratio is 1.0
- (D) Increase the PIP until the I/E ratio is 1:2
- (E) Increase the PIP to 50 cmH20
A 35-year-old woman with severe myasthenia gravis is scheduled for thymectomy. Which of the following preoperative pulmonary function tests is most likely to be normal?
- (A) Forced expiratory volume in 1 second (FEV1)
- (B) Forced vital capacity (FVC)
- (C) FEV1/FVC
- (D) Maximum voluntary ventilation
- (E) Peak inspiratory force
After a gastric stapling procedure, a 150-kg woman is extubated and breathing spontaneously in the recovery room at a rate of 26/min and an FiO2 of 0.5. Arterial blood gas analysis shows PaO2 96 mmHg, PaCO2 44 mmHg, and pH 7.37. The parameter most closely related to her increased alveolar-arterial oxygen tension gradient is
- (A) decreased expiratory reserve volume
- (B) decreased minute volume
- (C) decreased residual volume
- (D) decreased total lung capacity
- (E) rapid respiratory rate
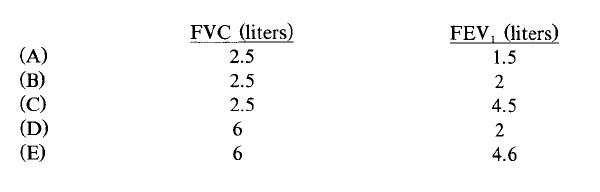
A 75-kg, 45-year-old patient with quadriplegia at the level of C6 is scheduled for elective cholecystectomy. Pulmonary function tests show an FVC of 2.4 L and an FEV, of 1.2 L. Which of the following is the most appropriate conclusion based on these findings?
- (A) Intercostal muscle function is normal
- (B) SpO, will be 80% or less while breathing room air
- (C) Total lung capacity is normal
- (D) The patient has chronic obstructive pulmonary disease
- (E) These findings are expected in this patient
Alveolar stability at varying lung volumes is maintained by
- (A) constant surface tension
- (B) increased surface tension at low lung volume
- (C) decreased surface tension at high lung volume
- (D) decreased surface tension at low lung volume
- (E) none of the above
Each of the following is a physiologic effect of intra-aortic balloon pump therapy EXCEPT
- (A) decreased peak systolic pressure
- (B) increased cardiac output
- (C) increased coronary perfusion
- (D) increased diastolic pressure
- (E) increased total peripheral resistance
Carbon monoxide poisoning with a carboxyhemoglobin concentration of 20% is characterized by each of the following EXCEPT
- (A) decreased oxygen-carrying capacity of hemoglobin
- (B) decreased PaO2
- (C) shift of the oxyhemoglobin dissociation curve to the left
- (D) normal minute volume of ventilation
- (E) headache and nausea
Compared with a person of normal weight, which of the following findings are most likely on pulmonary function testing of a patient with morbid obesity? (FVC, FEV/FVC, FRC, A-a DO2)?
- (A) Decreased, Normal, Decreased, Normal
- (B) Decreased, Normal, Decreased , Increased
- (C) Decreased, Normal, Normal, Increased,
- (D) Increased, Decreased, Normal, Increased
- (E) Increased, Decreased, Decreased, Increased
An obese, 70-year-old woman with a long history of tobacco abuse is awake and semirecumbent after uneventful anesthesia with isoflurane for a ventral hernia repair. During the first hour in the recovery room while breathing 50% oxygen by face mask, her arterial oxygen saturation decreases to 90% while other vital signs remain satisfactory. Which of the following is most likely to be effective in the management of this situation?
- (A) Intravenous doxapram
- (B) Racemic epinephrine by inhalation
- (C) Continuous positive airway pressure by mask
- (D) Reintubation of the trachea
- (E) Coughing
Which of the lines shown in the graph illustrates the relationship of hematocrit and oxygen transport?
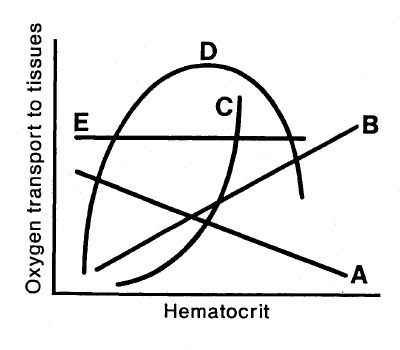
- (A) Line A
- (B) Line B
- (C) Line C
- (D) Line D
- (E) Line E
During right upper lobectomy and one-lung ventilation with a double-lumen endotracheal tube, the PaO2 decreases to 40 mmHg. The PaCO2 is 39 mmHg. Which of the following is most appropriate?
- (A) Confirm position of the tube with bronchoscopy
- (B) Apply 5 cmH20 continuous positive airway pressure to the nondependent lung
- (C) Apply 5 cmH20 positive end-expiratory pressure to the dependent lung
- (D) Resume two-lung ventilation
- (E) Clamp the pulmonary artery of the nondependent lung
A 35-kg child requires mechanical ventilation with pure oxygen at a tidal volume of 350 ml and a rate of 20/min during a severe asthma attack. The most likely cause of severe hypotension after initiating mechanical ventilation is
- (A) hypoxic circulatory depression
- (B) inadequate expiratory time
- (C) increased pulmonary vascular resistance
- (D) respiratory alkalosis
- (E) tension pneumothorax
A healthy, spontaneously breathing, supine, anesthetized patient has an arterial to end-tidal carbon dioxide tension difference of 3 mmHg. Following institution of mechanical ventilation the value increases to 12 mmHg. The most likely cause of this change is
- (A) cephalad displacement of the diaphragm
- (B) decreased production of carbon dioxide
- (C) increased cardiac output
- (D) increased shunting of blood through dependent lung zones
- (E) increased ventilation of nondependent lung zones
A patient with chronic obstructive pulmonary disease is undergoing spinal anesthesia to a T6 sensory level. The most pronounced effect on pulmonary function will be a decrease in
- (A) minute ventilation
- (B) peak expiratory flow
- (c) physiologic dead space
- (D) tidal volume
- (E) vital capacity
A 57-year-old man who weighs 150 kg and is 170 cm (67 in) tall is scheduled for cholecystectomy. He has a 100 pack-year smoking history. Which of the following findings on pulmonary function testing are most likely?
When compared with a healthy 30-year-old man, which of the following respiratory parameters is decreased in an otherwise healthy 80-year-old man?
- (A) Alveolar to arterial oxygen gradient
- (B) Lung compliance
- (C) Ratio of functional residual capacity to total lung capacity
- (D) Resting tidal volume
- (E) Ventilatory response to carbon dioxide
A 14-year-old girl with status asthmaticus is receiving oxygen 3 L/min through nasal prongs. Heart rate is 110 bpm. Arterial blood gas values are PaO2 90 mmHg, PaCO2 32 mmHg, and pH 7.46. If ventilation appears unchanged, which of the following is the most reliable sign of impending respiratory failure?
- (A) PaO2 of 80 mmHg
- (B) PaCO2 of 39 mmHg
- (C) Heart rate of 140 bpm
- (D) Increased wheezing
- (E) Deterioration of mental status
A 60-kg, 17-year-old girl with severe idiopathic scoliosis is scheduled for Harrington rod fixation. Which of the following respiratory parameters is compatible with this disorder?
- (A) Alveolar-to-arterial oxygen tension difference (A-aDO2) less than 100 mmHg while breathing pure oxygen
- (B) FEV1/FVC ratio less than 50%
- (C) Forced vital capacity less than 2000 ml
- (D) Intrapulmonary shunt less than 10%
- (E) Normal pulmonary vascular resistance
A 56-year-old woman with pulmonary fibrosis is scheduled for pneumonectomy. Which of the following parameters best predicts potential postoperative functional impairment?
- (A) Exercise tolerance
- (B) Flow-volume loop
- (C) Resting arterial blood gas values
- (D) Unilateral pulmonary artery occlusion pressure
- (E) Vital capacity and FEV,
Which of the following findings is most likely in an 85-kg 30-year-old man who is breathing spontaneously through 6-mm endotracheal tube?
- (A) Decreased PetCO2
- (B) Decreased SpO2
- (C) Increased minute ventilation
- (D) Increased respiratory rate
- (E) Increased tidal volume
A 70-kg, 77-year-old man Is undergoing left nephrectomy with nitrous oxide, oxygen, fentanyl, and midazolam anesthesia. He has a 90 pack-year history of cigarette smoking and has chronic obstructive pulmonary disease. One hour after incision, expiratory wheezing occurs and peak Inspiratory pressure increases from 35 to 65 cmH20; end-tidal PCO2 is unchanged, but SpO2 decreases from 97% to 88%. The most likely cause is
- (A) endobronchial intubation
- (B) overinflation of the endotracheal tube cuff
- (C) pneumothorax
- (D) pulmonary edema
- (E) pulmonary embolism
A 30-year-old man who is undergoing laparotomy and resection of a large kidney tumor has a decrease in SpO2 from 100% to 92% and an increase in peak airway pressure from 20 to 35 cm H2O. Plateau pressure is unchanged at 18 cm H2O. Which of the following is the most likely cause?
- (A) Abdominal packing
- (B) Inadequate anesthesia
- (C) Inadequate muscle relaxation
- (D) Obstruction of the endotracheal tube
- (E) Pneumothorax
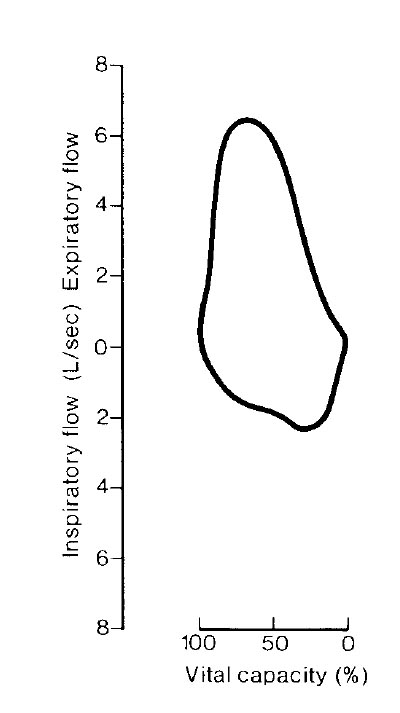
This flow-volume loop from a 57-year-old man is most consistent with which of the following conditions?
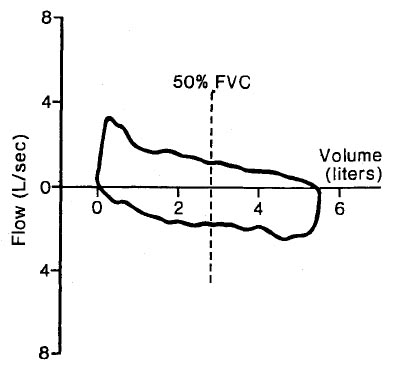
- (A) Bronchospasm
- (B) Decreased vital capacity
- (C) Myasthenia gravis
- (D) Narrowing of the upper airway
- (E) Pneumothorax
The sudden onset of pulmonary edema can be caused by each of the following EXCEPT
- (A) rapid re-expansion of the lungs following pneumothorax
- (B) upper airway obstruction
- (C) oxygen toxicity
- (D) rupture of mitral papillary muscle
- (E) severe preeclampsia
A 50-year-old man with an 80 pack-year history of cigarette smoking has a forced expiratory volume in one second of 1.5 L and a forced vital capacity of 3.5 L. Which of the following statements concerning intraoperative anesthetic management is true?
- (A) An I:E ratio of 1:1 will improve carbon dioxide removal more than an I:E ratio of 1:2.5
- (B) Antagonism of neuromuscular block will most likely trigger acute bronchospasm
- (C) Functional residual capacity will increase during an acute exacerbation of bronchospasm
- (D) Induction with ketamine will increase airway resistance
- (E) Nitrous oxide is contraindicated
High positive end-expiratory pressure can result in each of the following EXCEPT
- (A) decreased venous return
- (B) increased functional residual capacity
- (C) a left-to-right shift of the ventricular septum
- (D) decreased PaO2
- (E) pulmonary barotrauma
Which of the following provides the most definitive diagnosis in a patient with suspected brain death?
- (A) Absent bilateral somatosensory evoked potentials
- (B) Absent cerebral blood flow during four-vessel contrast cerebral arteriography
- (C) Intracranial pressure greater than mean arterial pressure
- (D) Score of zero on Glasgow Coma Scale
- (E) Two isoelectric electroencephalograms
A patient has decreased lung compliance and hypoxemia after a 30-minute episode of laryngospasm following extubation. The most likely cause is
- (A) allergic reaction to the anesthetic
- (B) altered alveolar-capillary membrane permeability
- (C) anesthetic-induced lymphatic dysfunction
- (D) increased pulmonary capillary pressure
- (E) negative pulmonary interstitial hydrostatic pressure
A 70-kg 22-year-old patient with head trauma and multiple fractures of the long bones is scheduled for fixation of bilateral femoral fractures. Preoperative laboratory studies show a serum sodium concentration of 150 mEq/L, a serum potassium concentration of 3.1 mEq/L, and a urine output greater than 500 ml/hr. Which of the following agents will decrease urine output?
- (A) 3% Saline solution
- (B) 5% Dextrose solution
- (C) Glucagon
- (D) Hydrocortisone
- (E) Vasopressin
Which of the following factors causes a decrease in mixed venous oxygen saturation?
- (A) Arteriovenous fistula
- (B) Decreased hemoglobin concentration
- (C) Decreased oxygen consumption
- (D) Increased cardiac output
- (E) Nitroprusside toxicity
A 52-year-old woman undergoes facial surgery during general endotracheal anesthesia. The ventilator is set to deliver a tidal volume of 600 ml and a respiratory rate of 10/min at an FiO2 of 1.0. SpO2 is 100%, peak inspiratory pressure is 18 cmH2O, and PetCO2 is 40 mmHg. The surgeon flexes the patient's head so the chin touches the chest. Which of the following findings indicates that endobronchial intubation has NOT occurred?
- (A) Fluctuating capnographic waveform
- (B) Greater expiratory volume than inspiratory volume
- (C) Unchanged SpO2
- (D) Unchanged PetCO2
- (E) Unchanged peak inspiratory pressure
During anesthesia, the ventilation/perfusion ratios change
- (A) to preferential ventilation of the dependent portion
- (B) due to cephalad shift of the diaphragm
- (C) by insignificant amounts from that in the awake state
- (D) to preferential perfusion of the superior portion
- (E) from changes in pulmonary compliance
Addition of 20 cmH2O positive end-expiratory pressure to a patient receiving controlled mechanical ventilation decreases cardiac output and left ventricular function by
- (A) increasing right ventricular preload
- (B) increasing right ventricular afterload
- (C) increasing left ventricular preload
- (D) increasing left ventricular afterload
- (E) producing myocardial ischemia
Microatelectasis 48 hours after abdominal surgery is most consistently manifested by
- (A) decreased PaO2
- (B) ground glass infiltrate on a roentgenogram of the chest
- (C) scattered fine inspiratory rales
- (D) increased PaCO2
- (E) scattered areas of dullness to chest percussion
During induction of general anesthesia in a patient with a supraglottic tumor, both intubation and subsequent ventilation via a face mask are impossible. A cricothyroidotomy is performed with a 16-gauge intravenous catheter. Which of the following statements is true?
- (A) Application of pressures greater than 35 cmH2O to the catheter will increase the risk for pulmonary barotrauma
- (B) PaC02 can be maintained at a normal level using a standard circle system attached to the catheter
- (C) PaO2 greater than 100 mmHg can be maintained indefinitely using transtracheal jet ventilation with pure oxygen through the catheter
- (D) Emergency surgical tracheostomy would have improved the likelihood of survival
- (E) The presence of this tumor contraindicates jet ventilation via cricothyroidotomy
During application of continuous positive airway pressure, lung compliance increases because of
- (A) decreased airway resistance
- (B) decreased lung water
- (C) decreased venous return
- (D) increased intercostal muscle tone
- (E) increased resting lung volume
During one-lung ventilation, each of the following affects hypoxic pulmonary vasoconstriction in the nonventilated lung EXCEPT
- (A) application of continuous positive airway pressure to the nonventilated lung
- (B) high alveolar pO2 in the ventilated lung
- (C) infusion of isoproterenol
- (D) low mixed venous pO2
- (E) pulmonary hypertension
A pulmonary artery catheter is placed in an awake patient breathing room air. Typical right ventricular and pulmonary artery pressure tracings are obtained. With the catheter balloon inflated, blood drawn from the distal port has a PaO2 of 100 mmHg, while a simultaneous radial artery sample has a PaO2 of 90 mmHg. These data indicate that the
- (A) shunt fraction is greater than 10%
- (B) catheter is in the wedged position
- (C) catheter has entered a pulmonary vein
- (D) cardiac output is abnormally high
- (E) oxygen electrode is malfunctioning
A 70-kg 24-year-old man with bilateral pneumonia whose lungs are being mechanically ventilated has the following measured parameters: tidal volume 750 ml; FiO2 0.7; rate 12/min; positive end-expiratory pressure 10 cmH2O; PaO2 75 mmHg; PaCO2 55 mmHg; pH 7.30. Which of the following alterations should be made in the ventilatory settings?
- (A) Decreasing positive end-expiratory pressure
- (B) Decreasing respiratory rate
- (C) Increasing fresh gas flow rate
- (D) Increasing FiO2
- (E) Increasing tidal volume
A comatose 40-year-old man is to undergo evacuation of an acute subdural hematoma. His left pupil is dilated and blood is present behind the left tympanic membrane. Each of the following is an acceptable intervention EXCEPT
- (A) application of 5 cm H20 positive end-expiratory pressure
- (B) blind nasotracheal intubation
- (C) use of isoflurane
- (D) use of nitrous oxide
- (E) use of succinylcholine
Which of the following changes is most likely in the patient whose pulmonary pathology is schematically illustrated?
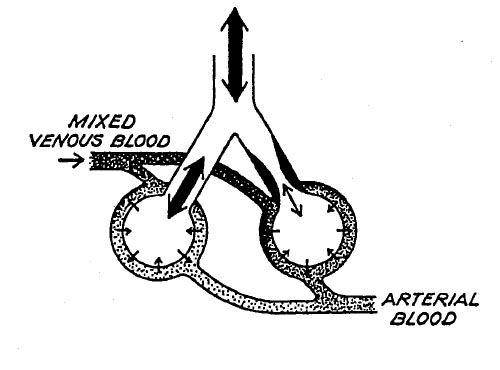
- (A) Decreased diffusing capacity
- (B) Decreased PaO2
- (C) Decreased pH
- (D) Increased PaCO2
- (E) Increased Vd/Vt
A 35-kg child requires mechanical ventilation with 100% oxygen at a tidal volume of 350 mL and a rate of 20/min during a severe asthma attack. The most likely cause of severe hypotension after initiating mechanical ventilation is
- (A) hypoxic circulatory depression
- (B) inadequate expiratory time
- (C) increased pulmonary vascular resistance
- (D) respiratory alkalosis
- (E) tension pneumothorax
Which of the following pulmonary components is altered the most in a morbidly obese patient?
- (A) Total lung volume
- (B) Tidal volume
- (C) Inspiratory reserve volume
- (D) Expiratory reserve volume
- (E) Ratio of dead space to tidal volume
A patient is scheduled for right pneumonectomy. A left-sided double-lumen endobronchial tube is inserted. After the endobronchial side is clamped and both cuffs are inflated, breath sounds are heard only on the left. Which of the following is the most likely cause?
- (A) Herniation of the endobronchial cuff over the carina
- (B) Occlusion of the right upper lobe bronchus
- (C) Placement of the endobronchial lumen in the left mainstem bronchus
- (D) Placement of the endobronchial lumen in the right mainstem bronchus
- (E) Placement of the endobronchial lumen in the trachea
A 90-kg, 59-year-old man with chronic obstructive pulmonary disease is undergoing laparotomy. Mechanical ventilation is being carried out with a fresh gas flow of 2 L/min at a rate of 16/min and tidal volume of 900 ml; I:E ratio is 1:2.5. PaCO2 remains greater than 50 mmHg. Preoperative PaCO2, was normal. Which of the following is the most appropriate next step?
- (A) Adding 10 cmH20 of positive end-expiratory pressure
- (B) Converting to spontaneous ventilation
- (C) Decreasing inspiratory flow rate
- (D) Increasing exhalation time
- (E) Increasing fresh gas flow
Compared with a patient who is breathing spontaneously, a patient in the supine position receiving controlled positive-pressure ventilation will most likely have which of the following findings?
- (A) Decreased pulmonary vascular resistance
- (B) Decreased ratio of dead space to tidal volume
- (C) Increased ventilation of nondependent alveoli
- (D) Increased perfusion of nondependent alveoli
- (E) Improved matching of ventilation to perfusion
A 54-year-old man is scheduled for open reduction of a fracture sustained when he jumped from a burning building. The carboxyhemoglobin concentration is 25%. Which of the following is the most reliable indicator of adequate oxygenation during general anesthesia?
- (A) PaO2 of 300 mmHg
- (B) pH of 7.38 with a PaCO2 of 41 mmHg
- (C) Mixed venous PO2 of 45 mmHg
- (D) Oxyhemoglobin saturation of 100% measured by co-oximeter
- (E) SpO2 of 100% measured by pulse oximeter
In a spontaneously breathing patient, each of the following increases the work of breathing EXCEPT
- (A) an increase in respiratory rate by 10/min
- (B) a decrease in lung-thorax compliance by 10 cmH2O
- (C) an increase in carbon dioxide production by 1 ml/kg/min
- (D) a decrease in PaO2 from 80 to 65 mmHg
- (E) a 0.1 increase in the ratio of dead space to tidal volume
Which of the following statements concerning pulmonary function in patients with pulmonary fibrosis is true?
- (A) Diffusion capacity is decreased
- (B) Pulmonary artery diastolic-to-occlusion pressure gradients are normal
- (C) Ventilation-perfusion relationships are normal
- (D) Static pulmonary compliance is unchanged
- (E) Mechanical ventilation with slow rate and large tidal volume is optimal
An acutely ill 65-year-old man with sepsis has severe hypophosphatemia. Which of the following is most likely to result from this electrolyte disorder?
- (A) Bronchospasm
- (B) Diarrhea
- (C) Muscle weakness
- (D) Seizures
- (E) Ventricular ectopy
In a patient with 20% pulmonary shunt and a PaO2 of 60 mmHg, cardiac output suddenly decreases from 5 L/min to 3 L/min. Oxygen consumption is unchanged. As a result, the PaO2 will
- (A) increase slightly because of decreased shunt blood flow
- (B) decrease slightly because of decreased mixed venous PO2
- (C) increase because of decreased affinity of hemoglobin for oxygen
- (D) decrease because of an increased dead space to tidal volume ratio
- (E) increase because of increased pulmonary oxygen uptake per milliliter of blood
In a patient with adult respiratory distress syndrome who is being mechanically ventilated, which of the following findings indicates the most severe disease?
- (A) Decreased functional residual capacity
- (B) Decreased lung compliance
- (C) Hypercarbia
- (D) Hypoxemia
- (E) Increased dead space
Which of the following statements about pulmonary function testing is true?
- (A) Forced expiratory volume in one second (FEV1) is directly related to maximum voluntary ventilation
- (B) FEV, is the most reliable indicator of small airways resistance
- (C) Forced vital capacity is markedly decreased in obstructive lung disease with air-trapping
- (D) Maximum mid-expiratory flow is less effort dependent than FEV1
- (E) Three-second forced expiratory volume is the amount of air exhaled during the third second of exhalation
Which of the following is the greatest disadvantage of pressure-cycled ventilation?
- (A) Increased I:E ratio
- (B) Increased mechanical dead space
- (C) Increased risk for barotrauma
- (D) Variable respiratory rates
- (E) Variable tidal volumes
A 55-year-old woman who is scheduled to undergo carotid endarterectomy has a history of essential hypertension and chronic obstructive pulmonary disease. Over a 30-minute period beginning one hour after induction of general anesthesia, Sp02 decreases from 99% to 95%. During that time, she has received fentanyl 100 mcg, isoflurane 1%, nitrous oxide 49.5%, oxygen 49.5%, and a nitroglycerin infusion to maintain blood pressure at approximately 160/95 mmHg. Which of the following is the most likely cause for the decline in oxygen saturation?
- (A) Decreased cardiac output
- (B) Increased dead space ventilation
- (C) Inhibition of hypoxic pulmonary vasoconstriction
- (D) Mainstem intubation
- (E) Second gas effect
Preoperative evaluation of a patient who has marked malnutrition will demonstrate each of the following EXCEPT
- (A) decreased respiratory muscle function
- (B) decreased serum albumin concentration
- (C) decreased metabolic rate
- (D) suppressed immune function
- (E) decreased extracellular fluid volume
A 50-year-old man who takes aspirin and nifedipine is scheduled for thoracotomy with one-lung ventilation. Which of the following is associated with the greatest risk for intraoperative hypoxemia?
- (A) Preoperative withdrawal of nifedipine therapy
- (B) Intraoperative mild respiratory acidosis
- (C) Intraoperative administration of isoflurane
- (D) Intraoperative administration of nitroglycerin
- (E) Intraoperative thoracic epidural morphine
Which of the following spirometric tests is most likely to be accurate in a patient with severe pain?
- (A) Forced expiratory volume in one second
- (B) Peak expiratory flow rate
- (C) Maximum midexpiratory flow
- (D) Maximum breathing capacity
- (E) Negative inspiratory pressure
If minute ventilation remains constant, a decrease in end-expiratory carbon dioxide concentration will occur with
- (A) a decrease in physiologic dead space
- (B) a decrease in cardiac output
- (C) a decrease in physiologic shunt fraction
- (D) the development of metabolic alkalosis
- (E) an increase in body temperature
A 120-kg 56-year-old man undergoing gastrectomy during anesthesia with fentanyl and isoflurane has a PetCO2 of 35 mmHg and a PaCO2 of 50 mmHg. His FEV,/FVC ratio is 80% of predicted. Heart rate is 120 bpm and arterial blood pressure is 80/40 mmHg. Which of the following is the most likely cause of the difference in PaCO2 and PetCO2?
- (A) Aspiration pneumonitis
- (B) Chronic obstructive pulmonary disease
- (C) Decreased cardiac output
- (D) Decreased VD/VT ratio
- (E) Increased QS/QT ratio
A 20-year-old man involved in a motor vehicle accident is brought to the operating room for irrigation and debridement of open fractures of the femur and humerus. Cyanosis, decreased breath sounds on the left, increased peak airway pressure, and hypotension are noted after intubation of the trachea. The most likely cause is
- (A) aspiration
- (B) fat embolus
- (C) intubation of the right mainstem bronchus
- (D) tension pneumothorax
- (E) unilateral bronchospasm
Two days after total abdominal hysterectomy, a 54-year-old woman develops lethargy followed by seizures and coma. Laboratory studies show a serum sodium concentration of 108 mEq/L and serum osmolality of 225 mOsm/kg. The most appropriate next step in management is administration of which of the following?
- (A) Desmopressin
- (B) Furosemide only
- (C) Saline solution 0.9% only
- (D) Furosemide and saline solution 0.9%
- (E) Furosemide and saline solution 3%
The primary purpose of denitrogenation prior to anesthetic induction is to
- (A) blunt hypoxic pulmonary vasoconstriction
- (B) improve ventilation and perfusion matching
- (C) increase contribution of second gas effect to rate of induction
- (D) increase oxygen reserve in the functional residual capacity
- (E) maximize arterial oxygen content
A 157 cm (5 ft 2 in), 180-kg, 40-year-old woman has a PaO2 of 65 mmHg, a PaCO2 of 38 mmHg, and a pH of 7.43 while breathing room air preoperatively. The most likely cause of these values is
- (A) decreased hypoxic ventilatory drive
- (B) higher than normal oxygen extraction from blood
- (C) lower than normal cardiac output
- (D) lower than normal functional residual capacity
- (E) polycythemia
A 64-year-old, 87-kg woman in good general health is undergoing a right knee arthroplasty while in the supine position with general anesthesia consisting of enflurane 2% and nitrous oxide 50% in oxygen. She is breathing spontaneously through a 7-mm endotracheal tube. During the first 30 minutes of the procedure, the arterial oxygen saturation measured by pulse oximetry decreases from 98% to 92%. The most likely cause of the desaturation is
- (A) decreased functional residual capacity
- (B) diffusion hypoxia
- (C) hypercarbia
- (D) increased airway resistance produced by the endotracheal tube
- (E) inhibition of hypoxic pulmonary vasoconstriction
Compared with intermittent positive pressure ventilation (IPPV), intermittent mandatory ventilation (IMV)
- (A) better maintains cardiac output
- (B) provides less than full mechanical ventilatory support
- (C) requires a greater level of sedation
- (D) requires a higher FlO2
- (E) requires a lower inspiratory flow rate
Which of the following is a cardiorespiratory effect of epidural block to a T4 sensory level?
- (A) Decreased expiratory reserve volume
- (B) Decreased tidal volume
- (C) Increased circulating catecholamine concentrations
- (D) Increased heart rate
- (E) Unchanged vital capacity
A patient sustains cardiac arrest while being mechanically ventilated. Which of the following is the most likely effect on PetCO2?
- (A) Gradual increase with the duration of asystole
- (B) Maintenance of the prearrest value
- (C) Abrupt decrease below the prearrest value
- (D) Decrease when thoracic compression is started
- (E) Gradual decrease independent of the ventilator cycle
Which of the following statements concerning pressure support ventilation is true?
- (A) It augments gas inflow in response to spontaneous inspiration
- (B) It increases inspiratory airway pressure during controlled mandatory ventilation
- (C) It requires the use of positive end-expiratory pressure
- (D) It functions independently of airway resistance/lung compliance
- (E) It correlates linearly with spontaneously achieved tidal volume
Static lung compliance is decreased by each of the following EXCEPT
- (A) pulmonary emphysema
- (B) congestive heart failure
- (C) adult respiratory distress syndrome
- (D) pulmonary fibrosis
- (E) inhalational anesthesia
Peak airway pressure increases from 25 to 50 cmH2O when beginning right endobronchial ventilation with a right double-lumen tube. The most likely explanation for this increase is
- (A) failure to decrease tidal volume
- (B) inadvertent intubation of the left mainstem bronchus
- (C) intrinsic resistance of small endobronchial lumina
- (D) obstruction of the orifice of the right upper lobe
- (E) overinflation of the bronchial tube cuff
Which of the following statements concerning carbon monoxide poisoning is true?
- (A) Diagnosis is excluded if the PaO2 is greater than 300 mmHg while breathing 100% oxygen
- (B) Increased inspired oxygen concentration accelerates displacement of carbon monoxide from hemoglobin
- (C) Methylene blue decreases binding of carbon monoxide to hemoglobin
- (D) Pulse oximetry accurately reflects hemoglobin oxygen saturation
- (E) Tissue oxygen delivery is normal
If minute ventilation remains constant, which of the following changes in PetCO2 and PaCO2 will result from a decrease in cardiac output? (PetCO2, PaCO2)
- (A) Decreased, Decreased
- (B) Increased, Increased
- (C) Unchanged, Unchanged
- (D) Decreased, Increased
- (E) Increased, Decreased
A patient receiving mechanical ventilation with oxygen 60% postoperatively has a PaO2 of 160 mmHg and a PaCO2 of 38 mmHg. One hour later, with mechanical ventilation unchanged, the PaO2 is 150 mmHg and PaCO2 is 48 mmHg. The most likely cause of these changes is
- (A) metabolic acidosis
- (B) pulmonary embolism
- (C) increased body temperature
- (D) interstitial pulmonary edema
- (E) aspiration pneumonia
Four hours after open cholecystectomy, a patient who is breathing spontaneously has an SpO2 of 93% in the supine position and an SpO2 of 98% when placed in the head-up position. The most likely cause of this change is an increase in which of the following?
- (A) Functional residual capacity
- (B) Minute ventilation
- (C) Pulmonary blood flow
- (D) Residual volume
- (E) Vital capacity
A child has tachypnea immediately after reintubation for intractable laryngospasm. Oxygen saturation is 78% at an FiO2 of 1.0. A radiograph of the chest taken 15 minutes later is most likely to show
- (A) bilateral pleural effusions
- (B) diffuse homogenous pulmonary infiltrates
- (C) patchy central infiltrates of the right upper lobe
- (D) pneumothorax
- (E) segmental atelectasis at both lung bases
During general anesthesia with spontaneous ventilation, a patient has a VD/VT of 0.5. Which of the following is most likely to decrease the ratio?
- (A) Acute bronchospasm
- (B) Continuous positive airway pressure
- (C) Decreased tidal volume
- (D) Increased cardiac output
- (E) Pulmonary embolism
A 29-year-old man who has been nasotracheally intubated for two weeks following a motor vehicle accident has a fever (39C) and a constant headache. Leukocyte count is 18,000/mm3. The most likely cause is
- (A) fractured nasal septum
- (B) retropharyngeal abscess
- (C) maxillary sinusitis
- (D) meningitis
- (E) rhinovirus infection