65 questions match your search.
Immediately after sustaining severe head injury, a 20-year-old man has a blood pressure of 150/90 mmHg and an intracranial pressure of 35 mmHg. After one hour of thiopental infusion, blood pressure is 105/60 mmHg, intracranial pres sure is 20 mmHg, central venous pressure is 5 mmHg, and temperature is 36°C. The EEG shows slow-wave activity. The most appropriate next step is administration of
- (A) additional thiopental
- (B) a corticosteroid
- (C) furosemide
- (D) nimodipine
- (E) phenylephrine
During Harrington rod instrumentation for scoliosis, monitoring somatosensory evoked potentials
- (A) is unreliable if halothane is used
- (B) eliminates the need for a wake-up test
- (C) accurately assesses proprioceptive integrity
- (D) accurately assesses motor function integrity
- (E) is unreliable if nondepolarizing muscle relaxants are used
Which of the following statements concerning postspinal headache is true?
- (A) Cerebrospinal fluid leukocytosis occurs
- (B) Intravenous caffeine therapy is more effective than epidural blood patch
- (C) The incidence decreases with age
- (D) The incidence is higher in males than in females of all ages
- (E) The incidence is the same after single or multiple dural punctures
The most important factor regulating blood flow to ischemic cerebral tissue is
- (A) systolic blood pressure
- (B) PaO2
- (C) cerebral perfusion pressure
- (D) PaCO2
- (E) cerebral oxygen consumption
Which of the following statements concerning brain stem auditory evoked responses is true?
- (A) They monitor cortical function
- (B) They are not affected by changes in carbon dioxide tension
- (C) They are not affected by mild hypothermia (34°C)
- (D) They are more resistant to anesthetic effects than somatosensory evoked responses
- (E) They are abolished coincident with flattening of the EEG
In patients with head trauma, which of the following factors results in a return of arterial pH toward normal levels after two days of mechanical hyperventilation?
- (A) Decreased renal absorption of hydrogen ions
- (B) Decreased renal blood flow
- (C) Increased PaCO2 with constant minute ventilation
- (D) Increased renal excretion of bicarbonate ions
- (E) Normalized cerebrospinal fluid pH
Which of the following is most likely to be effective in the treatment of clinically evident cerebral vasospasm occurring after subarachnoid hemorrhage?
- (A) Administration of nimodipine
- (B) Administration of thiopental
- (C) Decreasing cerebral perfusion pressure
- (D) Hypercarbia
- (E) Hypocarbia
A patient who is receiving ventilatory support after coronary artery bypass grafting has a PaO2 of 132 mmHg, a PaCO2 of 19 mmHg, and a pH of 7.57. Which of the following is most likely to result from this level of hypocarbia?
- (A) Decreased airway resistance
- (B) Increased myocardial contractility
- (C) Hyperkalemia
- (D) Shortened QT interval
- (E) Cerebral ischemia
In treating arterial hypertension in a patient with a head injury, the agent LEAST likely to increase intracranial pressure is
- (A) hydralazine
- (B) nitroprusside
- (C) nitroglycerin
- (D) trimethaphan
- (E) halothane
Cerebral blood flow is decreased by each of the following EXCEPT
- (A) etomidate
- (B) midazolam
- (C) nitrous oxide
- (D) increased minute ventilation
- (E) positive end-expiratory pressure
Monitoring sensory evoked potentials may be useful in detecting functional derangement of each of the following EXCEPT
- (A) cranial nerve pathways during posterior fossa operations
- (B) motor pathways during anterior cervical discectomy
- (C) dorsal column pathways during operations for spinal tumors
- (D) visual pathways during operations on the sphenoid wing
- (E) cortical pathways during carotid artery operations
Each of the following parameters of cerebral perfusion and metabolism is approximately equal to 50 EXCEPT
- (A) cerebral oxygen consumption in ml O2/min for a normal adult
- (B) lower limit of mean arterial pressure for cerebral autoregulation in mmHg
- (C) normal cerebral blood flow in ml /100 g tissue/min
- (D) PaO2 at which cerebral blood flow increases
- (E) PaCO2 at which cerebral blood flow doubles
Which of the following findings is most likely in patients with acute transection of the spinal cord at the level of C6?
- (A) Autonomic hyperreflexia
- (B) Hyperkalemia with administration of succinylcholine
- (C) Hypotension
- (D) Increased pulmonary blood flow
- (E) Tachycardia
Which of the following drugs increases cerebral blood flow while decreasing cerebral metabolic rate?
- (A) Etomidate
- (B) Fentanyl
- (C) Isoflurane
- (D) Lidocaine
- (E) Midazolam
In a patient receiving an epidural analgesic infusion postoperatively, clear fluid is noted to drip back freely from the epidural catheter. Each of the following findings correctly identifies the associated fluid EXCEPT
- (A) precipitation when mixed with an equal volume of thiopental — local anesthetic
- (B) pH 7.1— saline solution
- (C) glucose 55 mg/dl - CSF
- (D) sodium 150 mEq/L - CSF
- (E) PCO2 51 mmHg - CSF
A 35-year-old woman with a grade III subarachnoid hemorrhage is undergoing clipping of a middle cerebral artery aneurysm 48 hours after initial hemorrhage. Which of the following drugs used to induce hypotension is LEAST likely to affect intracranial pressure?
- (A) Esmolol
- (B) Hydralazine
- (C) Isoflurane
- (D) Nitroglycerin
- (E) Sodium nitroprusside
Which of the following can be used as a sole criterion for brain death?
- (A) Absence of cerebral blood flow
- (B) Absence of doll's eye movements
- (C) Fixed, dilated pupils
- (D) Isoelectric EEG
- (E) Unresponsiveness to all externally applied stimuli
A 55-year-old man has quadriplegia after undergoing suboccipital craniotomy in the sitting position for treatment of acoustic neuroma. Which of the following is the most likely cause?
- (A) Air embolism with the presence of a probe-patent foramen ovale
- (B) Compression of the cervical cord related to neck flexion
- (C) Jugular venous obstruction
- (D) Postoperative tension pneumocephalus
- (E) Sustained elevation of cerebral perfusion pressure
In a patient who is to undergo clipping of a cerebral aneurysm, an advantage of isoflurane over nitroprusside for induction of hypotension is
- (A) better maintenance of cardiac output
- (B) better maintenance of cerebral blood flow
- (C) greater decrease in cerebral oxygen consumption
- (D) greater decrease in afterload
- (E) more rapid titration of systemic blood pressure
Each of the following is an effect of rapid infusion of mannitol EXCEPT
- (A) depletion of electrolytes
- (B) impaired platelet adhesiveness
- (C) increased intracranial pressure
- (D) increased intravascular fluid volume
- (E) increased renal blood flow
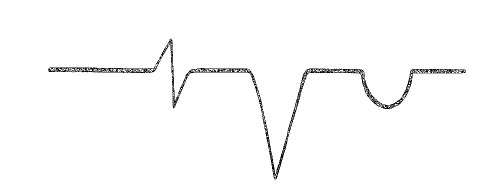
A 50-year-old patient is undergoing craniotomy for clipping of a cerebral aneurysm with isoflurane, nitrous oxide, and fentanyl anesthesia. At the time of aneurysm exposure, the EEG shows burst suppression. Which of the following is the most likely cause?
- (A) Cerebral ischemia
- (B) Cerebral vasospasm
- (C) Fentanyl effect
- (D) Isoflurane effect
- (E) Petit mal seizure activity
Which of the following provides the most definitive diagnosis in a patient with suspected brain death?
- (A) Absent bilateral somatosensory evoked potentials
- (B) Absent cerebral blood flow during four-vessel contrast cerebral arteriography
- (C) Intracranial pressure greater than mean arterial pressure
- (D) Score of zero on Glasgow Coma Scale
- (E) Two isoelectric electroencephalograms
Which of the following detects the smallest volume of venous air embolization?
- (A) Changing the precordial Doppler ultrasound signal
- (B) Decreasing PetC02
- (C) Decreasing Sp02
- (D) Increasing central venous pressure
- (E) Increasing pulmonary artery pressure
A radial artery catheter is to be used for blood pressure measurement during a sitting craniotomy. When zeroing the transducer, which of the following describes the best levels for placement of the transducer and opening of the system to air? (Transducer, Opening to Air)
- (A) Head Wrist
- (B) Head Head
- (C) Head Heart
- (D) Heart Heart
- (E) Heart Wrist
Which of the following would be most likely to increase the duration of seizures during electroconvulsive therapy using a barbiturate and succinyleholine for general anesthesia?
- (A) Administration of atropine prior to therapy
- (B) Changing to a benzodiazepine for induction
- (C) Changing to etomidate for induction
- (D) Adding phenytoin to preoperative medications
- (E) Decreasing the dose of barbiturate used for induction
Which of the following best describes the relationship between cerebral perfusion pressure and cerebral blood flow in a patient with untreated chronic hypertension?
- (A) It is constant at mean blood pressures between 50 and 150 mmHg
- (B) It is linear for all blood pressures
- (C) Flow versus pressure curve is hyperbolic
- (D) Flow versus pressure curve is shifted to the right
- (E) Flow versus pressure curve is shifted to the left
A 48-year-old woman underwent a posterior fossa craniotomy in the sitting position. Monitoring included precordial Doppler, arterial blood pressure, central venous pressure (CVP), and urine output. Furosemide was used intraopera-tively for cerebral decompression, and the operation was uneventful. In the recovery room, she was awake with stable vital signs when the CVP suddenly increased from 6 to 25 mmHg without any change in blood pressure. Shortly thereafter, premature ventricular contractions are noted. After administering lidocaine 1 mg/kg intravenously, the most appropriate action is to
- (A) position the patient head down, right side up and aspirate the CVP catheter
- (B) withdraw the CVP catheter 5 cm
- (C) infuse potassium chloride rapidly
- (D) administer furosemide
- (E) ask the neurosurgeon to reevaluate the patient immediately
A 50-year-old man is scheduled to undergo emergency craniotomy for evacuation of an epidural hematoma. His Glasgow Coma Scale score is 6; heart rate is 54 bpm, and blood pressure is 190/110 mmHg. The most appropriate initial management is administration of which of the following agents?
- (A) Atropine
- (B) Mannitol
- (C) Nimodipine
- (D) Sodium nitroprusside
- (E) Thiopental
A 4-month-old child undergoing a craniectomy for craniosynostosis is anesthetized with nitrous oxide and halothane. Suddenly the systolic blood pressure decreases from 75 to 30 mmHg, and the PetCO2 decreases from 35 to 6 mmHg. Which of the following maneuvers is LEAST likely to have a beneficial effect?
- (A) Administration of a fluid bolus
- (B) Administration of a vasopressor
- (C) Application of positive end-expiratory pressure
- (D) Discontinuation of nitrous oxide
- (E) Flooding the surgical wound with saline solution
Which of the following best reflects findings of inadequate cerebral perfusion during carotid cross clamping?
- (A) Decreased frequency on EEG
- (B) Increased latency of brain stem auditory evoked potentials
- (C) Increased spectral edge frequency
- (D) Jugular bulb oxygen tension of 27 mmHg
- (E) Stump pressure of 50 mmHg
Which of the following statements concerning brain stem auditory evoked responses is true?
- (A) They monitor cortical function
- (B) They are not affected by changes in PaCO2
- (C) They are not affected by mild hypothermia (34°C)
- (D) They are more resistant to anesthetic effects than somatosensory evoked responses
- (E) They are abolished coincident with flattening of the EEG
Which of the following drugs best facilitates management of cerebral vasospasm after subarachnoid hemorrhage?
- (A) Nifedipine
- (B) Nimodipine
- (C) Nitroglycerin
- (D) Nitroprusside
- (E) Thiopental
In patients with blunt head trauma, cerebral perfusion pressure is determined by the gradient between
- (A) diastolic pressure and central venous pressure
- (B) intracranial pressure and central venous pressure
- (C) mean arterial pressure and central venous pressure
- (D) mean arterial pressure and intracranial pressure
- (E) systolic pressure and intracranial pressure
A 62-year-old man is in the intensive care unit after successful craniotomy for excision of a meningioma. Blood volume is normal; laboratory studies show serum sodium concentration of 120 mEq/L, serum osmolality of 260 mOsm/L, urine sodium concentration of 50 mEq/L, and urine osmolality of 820 mOsm/L. Which of the following is the most likely explanation?
- (A) Fluid overload with 5% dextrose in water
- (B) Inappropriate secretion of antidiuretic hormone
- (C) Increased free water clearance
- (D) Nephrogenic diabetes insipidus
- (E) Neurogenic diabetes insipidus
During craniotomy in the sitting position, end-tidal carbon dioxide tension suddenly decreases. Ventilatory excursion of the chest is normal. Further evaluation is most likely to show a decrease in
- (A) alveolar-to-arterial oxygen tension difference
- (B) alveolar-to-arterial carbon dioxide tension difference
- (C) dead space ventilation
- (D) pulmonary artery pressure
- (E) pulmonary artery occlusion pressure
Intravenous administration of mannitol during a craniotomy
- (A) decreases intracranial pressure relative to dosage
- (B) hastens excretion of pancuronium
- (C) induces metabolic alkalosis
- (D) produces a sustained increase in intravascular volume
- (E) requires an intact blood-brain barrier to decrease brain water
A 30-year-old man who is breathing spontaneously has a ventilatory pattern of sustained deep inspiration and occasional expiratory gasps during emergence from general anesthesia after posterior fossa craniotomy. Which of the following is the most likely cause?
- (A) Air in the cerebral ventricles
- (B) Expiratory obstruction from subglottic edema
- (C) Injury to the C3-5 nerve roots
- (D) Injury to the pons
- (E) Residual neuromuscular paralysis
Depression of cerebral oxygen requirements below the level required to create an isoelectric EEG can be achieved by
- (A) administration of isoflurane
- (B) administration of nimodipine
- (C) barbiturate coma
- (D) hyperventilation
- (E) hypothermia
The EEG begins to flatten during carotid endarterectomy when regional cerebral blood flow (in ml/min/100 g brain) decreases to
- (A) 55
- (B) 45
- (C) 30
- (D) 20
- (E) 10
Prompt control of seizures induced by bupivacaine is necessary because
- (A) cerebral metabolic rate for oxygen increases more than cerebral blood flow
- (B) cerebral blood flow is increased
- (C) bupivacaine decreases aerobic cerebral metabolism
- (D) cardiac failure may occur
- (E) ventilation may be impaired
The most sensitive means of detecting venous air embolism is
- (A) precordial Doppler stethoscope
- (B) transesophageal echocardiography
- (C) end-tidal carbon dioxide measurement
- (D) pulmonary artery pressure measurement
- (E) central venous pressure measurement
Which of the following interventions is most effective in preventing neurologic injury resulting from global cerebral ischemia?
- (A) Induction of barbiturate coma prior to ischemia
- (B) Maintenance of serum glucose concentration greater than 200 mg/dl prior to ischemia
- (C) Induction of hypothermia to a core temperature of 15 degrees C prior to ischemia
- (D) Maintenance of PaCO2 less than 25 mmHg following ischemia
- (E) Prevention of systemic hypertension following ischemia
Cerebral blood flow is decreased by
- (A) chronic respiratory acidosis
- (B) hypoxia
- (C) hypoglycemia
- (D) polycythemia
- (E) the postictal state
Which of the following best explains the decreased effect of hyperventilation on cerebral blood flow when PaCO2 decreases below 20 mmHg?
- (A) Maximal constriction of cerebral vessels
- (B) Decreased cerebral perfusion pressure
- (C) Decreased cerebral metabolic rate for oxygen
- (D) Increased cardiac output
- (E) Increased cerebrospinal fluid pressure
A neurologically intact 48-year-old woman is scheduled for removal of a parietal lobe arteriovenous malformation. The relative risk for complete resection is to be determined by a test occlusion of the feeding artery. Which of the following intraoperative monitoring techniques is most appropriate for this test?
- (A) Brain stem auditory evoked potentials
- (B) Cerebral blood flow using radioactive xenon
- (C) EEG
- (D) Evoked potentials elicited by stimulating the posterior tibial nerve
- (E) Transcranial Doppler
Brain stem auditory evoked potentials are most likely to be absent during which of the following?
- (A) Anesthesia with 1.5 MAC isoflurane
- (B) Barbiturate coma
- (C) Hypotension to a mean arterial pressure of 50 mmHg
- (D) Surgical retraction of the temporal lobe
- (E) Surgical traction on the pons
A multi-orifices right heart catheter is being positioned by EKG control prior to sitting craniotomy. The EKG tracing is obtained between the distal tip of the catheter and the right arm lead. The most appropriate next step is to
- (A) leave the catheter in place
- (B) advance the catheter 2 to 3 cm
- (C) withdraw the catheter 2 to 3 cm
- (D) remove the catheter completely
- (E) change polarity of the EKG
An otherwise healthy 16-year-old girl is undergoing posterior spinal fusion for thoracolumbar scoliosis. During the procedure, the most likely cause of a marked decrease in the amplitude of the somatosensory evoked potentials after stimulation of the posterior tibial nerve is
- (A) administration of fentanyl 30 jag /kg for induction
- (B) administration of isoflurane 1.3 MAC for maintenance
- (C) administration of vecuronium 0.15 mg/kg
- (D) a decrease in body temperature from 37 to 35°C
- (E) a decrease in cerebrospinal fluid pressure
During a craniotomy for a supratentorial tumor, a 28-year-old man receives isoflurane 0.75% in nitrous oxide 70% and oxygen. Ventilation is controlled to maintain PaCO2 at 25 mmHg. Nasopharyngeal temperature is 35.8°C. While the dura mater is open, the surgeon complains that the brain is bulging. The most appropriate management at this time is to
- (A) decrease the inspired isoflurane concentration to 0.5%
- (B) hyperventilate further to decrease PaCO2 to 20 mmHg
- (C) discontinue nitrous oxide
- (D) administer thiopental
- (E) administer additional muscle relaxants
A 6-year-old boy undergoes craniotomy in the supine position for brain tumor during anesthesia with 1.5% isoflurane in oxygen. PetCO2 is 38 mmHg, heart rate is 78 bpm, and blood pressure is 130/80 mmHg. After opening the dura, the surgeon notes that the brain is bulging. Which of the following management options is LEAST likely to significantly decrease brain size?
- (A) Decreased isoflurane concentration
- (B) Furosemide
- (C) Hyperventilation to a PaCO: of 25 mmHg
- (D) Mannitol
- (E) Nitroprusside
A comatose 40-year-old man is to undergo evacuation of an acute subdural hematoma. His left pupil is dilated and blood is present behind the left tympanic membrane. Each of the following is an acceptable intervention EXCEPT
- (A) application of 5 cm H20 positive end-expiratory pressure
- (B) blind nasotracheal intubation
- (C) use of isoflurane
- (D) use of nitrous oxide
- (E) use of succinylcholine
The most likely cause of bilateral fixed and dilated pupils after clipping of a basilar artery aneurysm is
- (A) preoperative administration of atropine
- (B) intraoperative infusion of trimethaphan
- (C) naloxone antagonism of opioid
- (D) persistent hypothermia
- (E) brain stem ischemia
Each of the following statements about the blood supply of the spinal cord is true EXCEPT:
- (A) The anterior spinal artery is made up of branches from the vertebral, intercostal, and iliac arteries
- (B) The segmental blood supply of the cord depends upon the location of the arteria radicularis magna (Adamkiewicz)
- (C) The posterior spinal arteries supply most of the spinal cord
- (D) Obstruction of the inferior vena cava increases blood flow through the epidural venous plexus
- (E) The spinal cord is supplied by one anterior spinal artery and two posterior spinal arteries
Massive venous air embolism occurs in a patient who is undergoing craniotomy in the sitting position with nitrous oxide, oxygen, fentanyl anesthesia. Which of the following changes in end-tidal (ET) concentrations of carbon dioxide, nitrogen, and nitrous oxide are most likely in this patient? (ETCO2, ETN2, ETN2O)
- (A) Increased, increased, decreased
- (B) Decreased, decreased, increased
- (C) Decreased, decreased, decreased
- (D) Decreased, increased, decreased
- (E) Increased, decreased, decreased
One hour after induction of anesthesia for a posterior fossa craniotomy using opioid, relaxant, and nitrous oxide, the brain begins to protrude through the dura. The most effective measure to decrease intracranial pressure is to
- (A) administer additional opioid
- (B) decrease PaCO2 from 25 to 15 mmHg
- (C) drain cerebrospinal fluid
- (D) discontinue nitrous oxide
- (E) induce hypotension
In a healthy patient receiving an epidural analgesic infusion postoperatively, clear fluid is noted to drip back freely from the epidural catheter. Which of the following findings correctly identifies the associated fluid?
- (A) Precipitation when mixed with an equal volume of pancuronium = local anesthetic
- (B) pH 7.1 = saline solution
- (C) Glucose 120 mg/dl = CSF
- (D) Sodium 130 mEq/L = CSF
- (E) PCO2 51 mmHg = CSF
Which of the following statements concerning barbiturate protection from cerebral ischemia is true?
- (A) It may be achieved with dosages low enough to avoid cardiovascular effects
- (B) It is linearly dose-related
- (C) It improves neurologic outcome following cardiac arrest
- (D) It is most useful in patients with focal ischemia
- (E) It is unrelated to EEG activity
A middle-aged, 70-kg man with a brain tumor is scheduled for an elective craniotomy. Preoperatively, he is alert but papilledema is present. Anesthesia is induced with thiopental 300 mg and succinylcholine 100 mg, followed by tracheal intubation. Immediately following intubation vigorous bucking occurs. The best immediate management would be to
- (A) administer succinylcholine 100 mg intravenously
- (B) administer fentanyl 500 jug intravenously
- (C) hyperventilate with isoflurane 2%
- (D) administer thiopental 400 mg intravenously
- (E) hyperventilate and administer lidocaine 1 mg/kg intravenously
A 70-kg, 46-year-old man is undergoing clipping of a cerebral aneurysm with nitrous oxide, opioid, relaxant anesthesia. He is otherwise healthy. As the surgeons are about to enter the dura, the brain is noted to be tense and bulging. Heart rate is 100 bpm and mean arterial pressure is 90 mmHg. PaO2 is 120 mmHg, PaCO2 is 23 mmHg, and pH is 7.50. Which of the following should be done immediately?
- (A) Hyperventilation to a PaCO2 of 15 to 20 mmHg
- (B) Administration of furosemide 20 mg intravenously
- (C) Administration of mannitol 0.5 g/kg
- (D) Administration of thiopental 250 mg in increments
- (E) Addition of halothane 1% to deepen anesthesia
A 32-year-old woman is anesthetized for suboccipital craniotomy. During positioning, the capnograph shows an abrupt decrease in the slope of the expiratory upstroke. Which of the following is the most likely cause?
- (A) Air embolism
- (B) Incompetent expiratory valve
- (C) Incomplete neuromuscular block
- (D) Kinked endotracheal tube
- (E) Tracheal extubation
A patient suddenly makes a respiratory effort during craniotomy for clipping of a cerebral aneurysm in a 15-degree head-up position with controlled ventilation. The most likely cause is
- (A) air embolism
- (B) cerebral hypoxia
- (C) direct stimulation of the respiratory center
- (D) intraventricular hemorrhage
- (E) stimulation of the motor cortex
Which of the following statements concerning air embolism during intracranial operations is true?
- (A) It does not occur in supine patients
- (B) It is prevented by positive end-expiratory pressure
- (C) It is confined to the right side of the heart and the pulmonary vasculature
- (D) It is detectable by measurement of end-tidal nitrogen
- (E) It is most efficiently treated by aspiration from a pulmonary artery catheter
The following changes occur during posterior cervical fusion in the prone position under halothane and nitrous oxide anesthesia with mechanical ventilation: HR 78 --> 84 with frequent PVCs; BP 110/70 --> 90/50; EtCO2 4.5% --> 2.0%; EtN2 0.12% --> 4% The most appropriate next step is to
- (A) administer lidocaine intravenously
- (B) decrease ventilatory rate
- (C) discontinue halothane
- (D) lower the patient's head
- (E) inspect the ventilator bellows
A 45-year-old woman who sustained a subarachnoid hemorrhage 18 hours ago develops a severe headache and becomes unresponsive. Which of the following is the most likely cause of this patient's change in mental status?
- (A) Cerebral edema
- (B) Cerebral embolism
- (C) Cerebral vasospasm
- (D) Hypertensive encephalopathy
- (E) Second subarachnoid hemorrhage
Deliberate hypothermia and circulatory arrest is planned for clipping of a giant basilar artery aneurysm. Which of the following statements is true?
- (A) Administration of a muscle relaxant slows the cooling process
- (B) Anesthesia is not required if body temperature is below 31°C
- (C) Decreasing body temperature below the level at which the EEG is isoelectric further decreases cerebral metabolic rate for oxygen
- (D) Sinus bradycardia during cooling results from increased intracranial pressure
- (E) T-wave inversion during cooling indicates myocardial ischemia